Introduction
Disease monitoring in management of acute leukemia is essentially important in terms of risk stratification and assessing response to chemotherapy throughout the disease course for which minimal residual disease (MRD) testing is the most reliable tool. Measurement of MRD by flow cytometry is based on the principle of studying difference in antigenic expression of the leukemic cells, hematogones and residual normal B cells. Modulation of antigen expression is an established fact that occurs on leukemic blasts during treatment under the influence of chemotherapeutic drugs, which may cause difficulty in analysis and detection of MRD [H.Burnusuzov et al. Folia Medica 2016;58(1):28-35]. Literature has reported antigen expression modulation, particularly during the glucocorticoid phase of induction therapy [Dworzak et al. Cytometry Part B 2010; 78B: 147-153]. For MRD assessment, such phenotypic shifts pose a particular challenge since they can cause misinterpretations and false results. However to our knowledge there hasn't been a large cohort studied to map antigenic modulation and analyze similar antigenic trends in comparison between leukemic blasts and non-leukemic B cells which may coexist during different phases of chemotherapy.
Key words: B-lymphoblastic leukemia, Flowcytometry, Antigen modulation, Minimal residual disease, Immunophenotype
Methods:
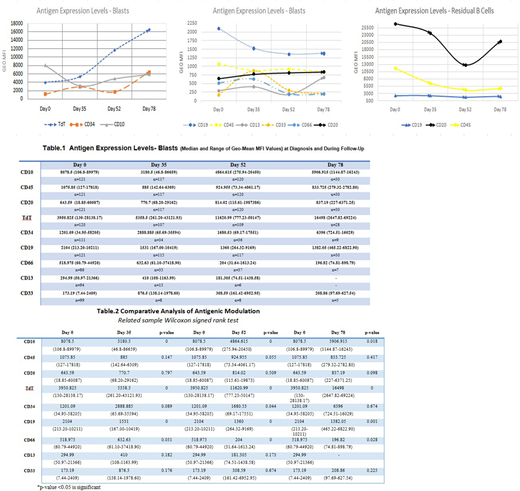
The study is conducted at the Hematology department of The Indus Hospital from April 2018 to March 2020. Among 445 pediatric B-lymphoblastic leukemia patients (1 month-18 years); we studied 121 patients who were MRD positive in bone marrow throughout the evaluation period. All patients received Berlin-Frankfurt-Munster (BFM) chemotherapy protocol as per National Cancer Institute (NCI) risk stratification criteria. To observe immunophenotypic modulation (IM) in antigen expression of Tdt, CD34, CD10, CD20, CD45, CD13, CD33 and CD66, compared from the time of diagnosis (day 0), post induction chemotherapy (day 35), post consolidation chemotherapy (day 52) and during maintenance chemotherapy (day78). Using eight color Flowcytometry (BD FACS CANTO-II; DIVA software version 8.0.2), the IM was assessed by comparative analyses of the changes in the mean flourescence intensity (MFI) of leukemic and non-leukemic B cells. The Wilcoxon signed rank test is used to compare median of MFI values at diagnosis and subsequent time points of MRD. Independent sample T-test/Mann-Whitney U test was applied as appropriate to determine significant differences in expression of antigens. A p-value of < 0.05 was considered as significant. Box and whisker plots and run charts will be used for descriptive purposes.
Results:
Mean age of the patients was 5.7years ±3.7 with male to female 1.7:1.We analyzed forward scatter and side scatter properties and antigen expression of the leukemic and normal residual B-cells. We observed statistically significant differences in MFI levels of CD10, CD20, CD19, CD45, CD66 and Tdt of leukemic cells showing trends at different phases. Down modulation of CD10 was noticed from day 0-day 35 however up modulation was observed in subsequent phases. CD20 and TdT both showed significant and stable up modulation from day 0-day78. A steep down modulation was observed in CD45 and CD19 from day 0 to day 52 and thereafter remained stable. CD34 expression was variable and showed up modulation at day 35 followed by down modulation and then again a reincrease at day 78. CD66, CD33 and CD13 showed similar varying trends exhibiting up modulation at day 35 and then down modulation at day 52 and day 78. Residual normal B cells showed substantial decrease in antigenic expression for CD19, CD20 and CD45 till day 52 followed by an ascent at day 78.
Conclusion:
Immunophenotypic modulation occurred to different extents in all analyzed samples. Our results confirm the presence of transient immunophenotypic changes for CD10, CD34, CD13, CD33 and CD66 at induction phase of chemotherapy whereas CD20 and TdT showed irreversible gain in expression that is exploitable for MRD detection. The MFI of the different antigens expressed by the leukemic blasts should be taken into consideration and cautiously analyzed for MRD detection.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.